Vomiting in early pregnancy: when it isn't normal
By Dr. Goh Shen Li
Obstetrician & Gynaecologist
MBBS, FRCOG (London), FAMS (Singapore)
The majority of pregnant women experience some degree of nausea and vomiting (70–80%) in the first trimester of pregnancy. Its severity can vary from person to person and even during different pregnancies in the same woman.
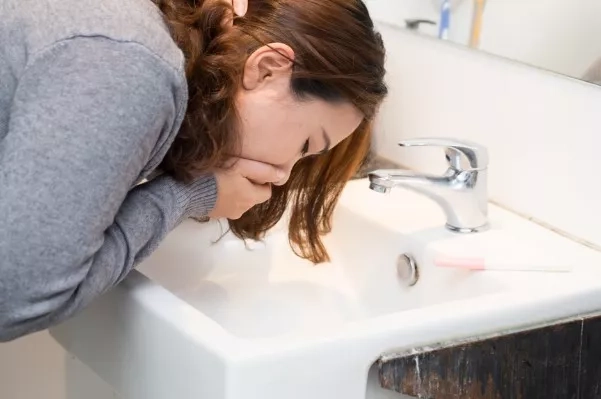
When the vomiting is severe
Hyperemesis gravidarum (HG) is a condition in pregnancy characterized by extreme nausea, excessive vomiting, weight loss and dehydration, and even fluid and electrolyte imbalances. It affects up to 2–3% of pregnant women.
People don't get HG very often, but nausea and vomiting are common during pregnancy, so it can be hard to tell the difference between this and the more common pregnancy sickness. (PRODIGY 2008, Festin 2009, HER 2010, Matthews et al 2010, Ogunyemi and Fong 2009) HG usually begins at between 6 and 7 weeks of pregnancy (HER 2010), easing off at 14 to 16 weeks of pregnancy. In many cases, HG will end by 20 weeks of pregnancy. Very few sufferers have symptoms that last the whole pregnancy.
How do I know if this is normal or not?
If you have HG, self-help treatments cannot help much and you feel miserable. You are exhausted and are unable to enjoy the pregnancy. You struggle with day-to-day life and are unable to eat and drink. You find it difficult to swallow your own saliva without vomiting (Ogunyemi and Fong 2009, Suzuiki et al. 2009, HER 2010). You vomit several times a day, and you are losing weight.
Recognise the following signs and symptoms - (HER 2010)
- Loss of 5% or more of pre-pregnancy body weight
- Dehydration, causing metabolite disturbances and constipation
- Nutritional disorders such vitamin deficiencies
- Physical and emotional stress of pregnancy on the body
- Difficulty with activities of daily living
- Severe nausea and vomiting
- Food aversions
- Decrease in urination
- Headaches
- Confusion/ fainting
- Jaundice
- Extreme fatigue
- Low blood pressure
- Rapid heart rate
- Loss of skin elasticity
- Secondary anxiety/depression
Hunger, tiredness, prenatal vitamins (especially those with iron), and diet can all make symptoms worse. Some women with HG lose as much as 10% of their body weight. They are also very sensitive to smells around them, and some smells can make their symptoms worse.
| Morning Sickness: | Hyperemesis Gravidarum: |
| Nausea sometimes accompanied by vomiting | Nausea accompanied by severe vomiting |
| Nausea that subsides at 12 weeks or soon after | Nausea that does not subside |
| Vomiting that does not cause severe dehydration | Vomiting that causes severe dehydration |
| Vomiting that allows you to keep at least some food down | Vomiting that does not allow you to keep any food down at all |

Why does this happen?
There are theories that suggest HG is due to a combination of factors, which may vary among women and include genetics, body chemistry, and overall health.
One theory is an adverse reaction to the hormonal changes of pregnancy. This would explain why HG happens most often in the first trimester (often between 8 and 12 weeks of pregnancy), when the levels of the pregnancy hormone (hCG) are the highest. Another postulation is an increase in maternal levels of female hormones in the body, leading to slower digestion and delayed passage of food from the stomach to the intestines, thus increasing the nausea and vomiting.
Risk factors for HG
- Hyperemesis gravidarum during a previous pregnancy
- Being overweight
- Having a twin pregnancy
- Being a first-time mother or young mother
- Being prone to motion sickness or migraines
- Pre-existing liver disease
- The presence of trophoblastic disease, which involves the abnormal growth of cells inside a woman's uterus e.g. molar pregnancy
Will my baby be in danger?
HG is physically and emotionally stressful, but it is also important to know that if it is treated, it is extremely unlikely that your baby will be malnourished or harmed (PRODIGY 2008, Festin 2009). Most studies show no health or developmental differences between infants of women who experienced the condition and those who did not.
If you lose weight during your pregnancy, there is an increased risk that the birthweight of the baby may be less than average. However, almost all women regain the weight they had lost in the early stages of pregnancy, usually during the second trimester, and go on to put on enough weight by the time of delivery.
Management of HG - what can be done?
- There is no known prevention of HG but you can take comfort in knowing that there are ways to manage it. All drugs should be used with care in pregnancy, especially in your first trimester, but many anti-nausea medications have a good safety record and have not been shown to have ill-effects on babies (PRODIGY 2008). Consider asking your doctor for anti-nausea medications to help you cope.
- Mild cases are treated with dietary changes, rest and oral medications. More severe cases often require a stay in the hospital so that the mother can receive fluid and nutrition through an intravenous line (IV).
Treatment depends on how ill a woman is and might include:
- Trying vitamin B6, and/or ginger.
- Small frequent meals—Nausea and vomiting might be treated with dry foods (such as crackers), small frequent meals and emotional support.
- Intravenous (IV) fluids—It is important for a pregnant woman to maintain her fluid intake. IV fluids might be needed if a woman continues to vomit throughout the pregnancy or does not improve with oral medications. In severe cases, hospitalisation is required for continued IV fluids and vitamins can be added into the IV fluids. IV fluids might be discontinued when a woman is able to take in fluids by mouth.
- Medicines — Medication to reduce nausea is used when vomiting is so persistent that it may pose possible risks to the mother or baby. If a woman cannot take medicines by mouth, the drugs can be administered through an IV or a rectal suppository. Common medicines used to alleviate nausea include promethazine, metoclopramide, prochlorperazine, and dimenhydrinate. If you are also heaving gastric reflux, anti-reflux medications can be given together as well. (HER 2010)
- Doing urine and blood tests to monitor the degree of dehydration and electrolyte levels e.g. sodium and potassium, and if abnormal, corrected with supplementation.

What next?
After IV rehydration is completed, you can progress to frequent small liquids or bland meals. Treatment then focuses on managing symptoms to allow normal food intake. However, cycles of dehydration can recur, making continuing care or repeated hospitalization necessary. (NHS 2010)
- Stay hydrated by taking small sips of fluid, or by sucking ice cubes (NHS 2010) or lollipops.
- Eat whatever you can manage or like. Do not worry if it is not a balanced diet or your regular meal. You can always catch up on good nutrition later, as your baby will get her nourishment from your body’s current reserves.
- Tweaking your diet to eliminate fatty and spicy foods, which are more likely to cause nausea
- Avoiding smells or tastes that tend to set you of.
- If you do not have severe anemia, wait until the nausea has improved before starting iron supplements.
- Try natural remedies such as ginger and peppermint alongside medical treatments (NCCWCH 2008, Festin 2009)
- Get as much rest as you can. Tiredness can make nausea and vomiting worse (NHS 2010), and make you feel unable to cope with the pregnancy. (PRODIGY 2008)
Recent Blog Posts
- 01 Aug 2025
- 02 Jun 2025
- 28 Mar 2025
- 10 Nov 2023
- 19 Oct 2022
